- You are here:
- Home
- >
- Guidelines summaries
- >
- Respiratory
Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care
National Institute for Health and Care Excellence
Key priorities for implementation
Diagnose COPD
- A diagnosis of COPD should be considered in patients over the age of 35 who have a risk factor (generally smoking) and who present with exertional breathlessness, chronic cough, regular sputum production, frequent winter ‘bronchitis’ or wheeze
- The presence of airflow obstruction should be confirmed by performing post-bronchodilator spirometry. All health professionals involved in the care of people with COPD should have access to spirometry and be competent in the interpretation of the results
Stop smoking
- Encouraging patients with COPD to stop smoking is one of the most important components of their management. All COPD patients still smoking, regardless of age, should be encouraged to stop, and offered help to do so, at every opportunity
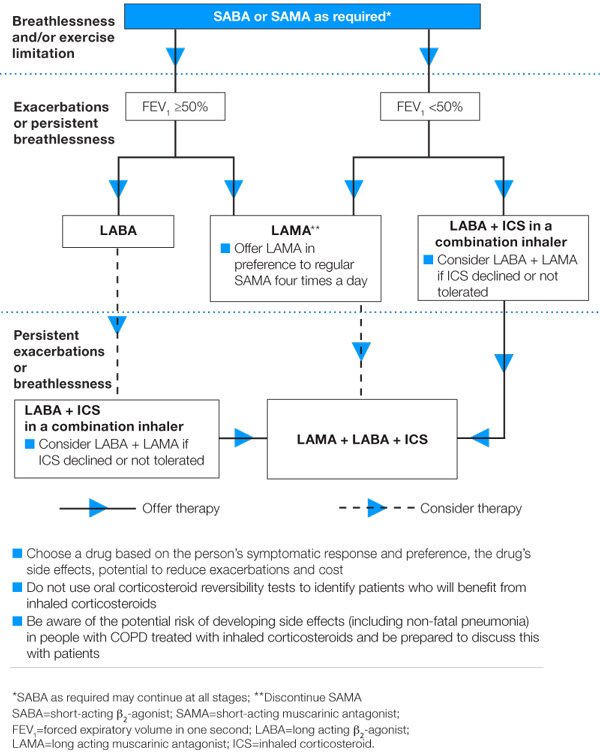
Promote effective inhaled therapy
- In people with stable COPD who remain breathless or have exacerbations despite use of short-acting bronchodilators as required, offer the following as maintenance therapy:
- if forced expiratory volume in 1 second (FEV1)≥50% predicted: either long-acting beta2 agonist (LABA) or long-acting muscarinic antagonist (LAMA)
- if FEV1<50% predicted: either LABA with an inhaled corticosteroid (ICS) in a combination inhaler, or LAMA
- Offer LAMA in addition to LABA + ICS to people with COPD who remain breathless or have exacerbations despite taking LABA + ICS, irrespective of their FEV1
Provide pulmonary rehabilitation for all who need it
- Pulmonary rehabilitation should be made available to all appropriate people with COPD including those who have had a recent hospitalisation for an acute exacerbation
Use non-invasive ventilation
- Non-invasive ventilation (NIV) should be used as the treatment of choice for persistent hypercapnicventilatory failure during exacerbations not responding to medical therapy. It should be delivered by staff trained in its application, experienced in its use and aware of its limitations
- When patients are started on NIV, there should be a clear plan covering what to do in the event of deterioration and ceilings of therapy should be agreed
Manage exacerbations
- The frequency of exacerbations should be reduced by appropriate use of inhaled corticosteroids and bronchodilators, and vaccinations
- The impact of exacerbations should be minimised by:
- giving self-management advice on responding promptly to the symptoms of an exacerbation
- starting appropriate treatment with oral steroids and/or antibiotics
- use of non-invasive ventilation when indicated
- use of hospital-at-home or assisted-discharge schemes
Ensure multidisciplinary working
- COPD care should be delivered by a multidisciplinary team
Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care continued
Managing symptoms and conditions in stable COPD
Breathlessness and exacerbations
- Manage breathlessness and exercise limitation with inhaled therapy
- For exacerbations or persistent breathlessness:
- use long-acting bronchodilators or LABA + ICS
- consider adding theophylline if still symptomatic
- Offer pulmonary rehabilitation to all suitable people
- Refer patients who are breathless, have a single large bulla on a CT scan and an FEV1 less than 50% predicted for consideration of bullectomy
- Refer people with severe COPD for consideration of lung volume reduction surgery if they remain breathless with marked restrictions of their activities of daily living, despite maximal medical therapy (including rehabilitation), and meet all of the following:
- FEV1 greater than 20% predicted
- PaCO2 less than 7.3 kPa
- upper lobe predominant emphysema
- TLCO greater than 20% predicted
- Consider referring people with severe COPD for assessment for lung transplantation if they remain breathless with marked restrictions of their activities of daily living despite maximal medical therapy. Considerations include:
- age
- FEV1
- PaCO2
- homogeneously distributed emphysema on CT scan
- elevated pulmonary artery pressures with progressive deterioration
- comorbidities
- local surgical protocols
Frequent exacerbations
- Optimise inhaled therapy
- Offer vaccinations and prophylaxis
- Give self-management advice
- Consider osteoporosis prophylaxis for people requiring frequent oral corticosteroids
Cor pulmonale
- Consider in people who have peripheral oedema, a raised venous pressure, a systolic parasternal heave, a loud pulmonary second heart sound
- Exclude other causes of peripheral oedema
- Perform pulse oximetry, ECG and echocardiogram if features of cor pulmonale
- Assess need for LTOT
- Treat oedema with diuretic
- Angiotensin-converting enzyme inhibitors, calcium channel blockers, alpha-blockers are not recommended
- Digoxin may be used where there is atrial fibrillation
Respiratory failure
- Assess for appropriate oxygen
- Consider referral for assessment for long-term domiciliary NIV therapy
Abnormal BMI
- Refer for dietetic advice
- Offer nutritional supplements if the BMI is low*
- Pay attention to weight changes in older patients (especially>3 kg)
Chronic productive cough
- Consider mucolytic therapy
Anxiety and depression
- Screen for anxiety and depression using validated tools in people who:
- are hypoxic
- are severely breathless or
- have recently been seen or treated at a hospital for an exacerbation
- Refer to ‘Depression with a chronic physical health problem’ (NICE clinical guideline 91).
Alpha-1 antitrypsin deficiency
- Offer referral to a specialist centre to discuss the clinical management of this condition
- Alpha-1 antitrypsin replacement therapy is not recommended
Palliative setting
- Opioids should be used when appropriate for the palliation of breathlessness in people with end-stage COPD unresponsive to other medical therapy
- Use benzodiazepines, tricyclic antidepressants, major tranquillisers and oxygen to treat breathlessness
- Provide access to multidisciplinary palliative care teams and hospices
Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care continued
Inhaled therapy
* See ‘Nutrition support in adults’ (NICE clinical guideline 32).
full guideline available from…
National Institute for Health and Care Excellence, Level 1A, City Tower, Piccadilly Plaza, Manchester, M1 4BT
guidance.nice.org.uk/CG101
National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease: management of chronic pulmonary disease in adults in primary and secondary care. Quick reference guide.. June 2010
- Continue reading:
- 1
- 2
- 3
- Next →
Please to rate this article, view others comments or make your own.

eGuidelines.co.uk (30 June 2013)
© 2013
First included: Jun 10.
disclaimer |



